Too often left with limited treatment options and time, patients with mesothelioma know too well the devastating effects of this aggressive disease. Many patients (41.5%) don’t advance to second-line therapy, according to a study from the University of California, San Diego.1

This “survival cliff” underscores a pressing need to expand treatment options to help prevent patients from falling through the cracks. Anne Tsao, MD, MBA, explored how administering chemotherapy and immunotherapy (chemo-IO) combinations in the frontline could help overcome this challenge during a debate at the Targeted Therapies in Lung Cancer Meeting in Huntington Beach, California. The debate and other meeting coverage will be available on demand for registered attendees via the IASLC Lung Cancer 360.
“We need faster tumor cytoreduction and higher objective response rates,” Dr. Tsao said. “That’s how we get patients over that [cliff] and transition them to subsequent lines of therapy.”
Dr. Tsao shared the scientific rationale and basis for chemo-IO in mesothelioma.
“In essence, you’re priming the immune system, overcoming the immunosuppressive tumor microenvironment. You also have the potential to induce long-term immunity by switching some of these cold tumors, which have low T-cell infiltration, into hot tumors,” she said.
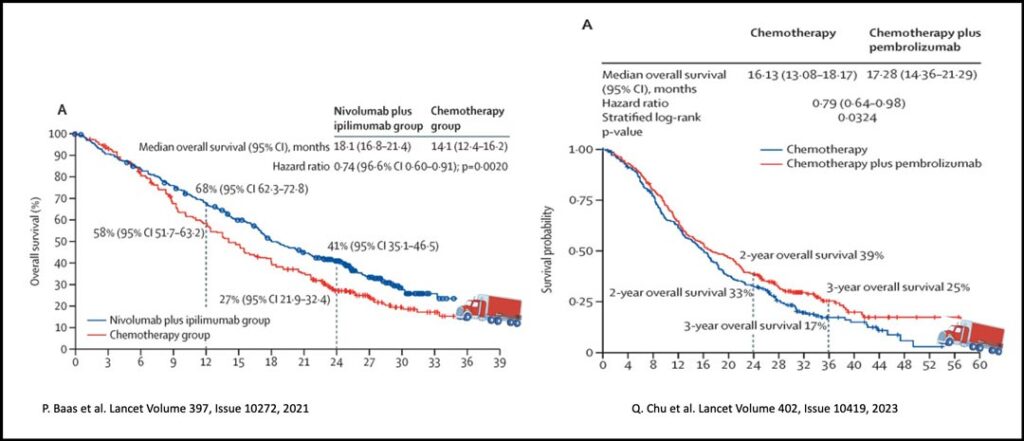
Dr. Tsao shared data from well-known clinical trials supporting chemo-IO: IND227, BEAT-Meso, and CheckMate 743.
IND227 compared chemotherapy alone to chemotherapy combined with pembrolizumab in patients with mesothelioma. The trial results indicated a clear benefit for the chemotherapy-pembrolizumab group with overall survival (OS) of 17.3 months versus 16.1 months for the chemotherapy group.
Dr. Tsao noted that while this OS benefit was predominantly observed in patients with non-epithelioid mesothelioma, those with epithelioid mesothelioma still achieved a numerically higher median OS of 19.8 months with chemotherapy plus pembrolizumab, compared with 18.2 months for chemotherapy alone.
“Without a doubt, there’s always going to be a greater magnitude of benefit when using IO therapies in patients with non-epithelioid histology,” Dr. Tsao said. “But that does not negate the fact that some patients with epitheliod disease also derive significant survival benefits.”
The BEAT-Meso trial, which added bevacizumab to chemotherapy and atezolizumab, also demonstrated favorable OS benefits (20.5 months for chemotherapy with bevacizumab and atezolizumab versus 18.1 months for chemotherapy with bevacizumab).
Again, while the OS benefit was more significant in the non-epithelioid cohort, PFS improvement was observed across all histologic subtypes.
Lastly, Dr. Tsao shared updated results from the CheckMate 743 trial, which compared a combination of ipilimumab and nivolumab to combination platinum and pemetrexed. While there was an OS benefit for the ipilimumab plus nivolumab cohort (68% versus 58% at 12 months), there was no significant PFS benefit, with a median PFS of 6.8 months versus 7.2 months.
However, Dr. Tsao noted that the response rates were similar (40% for ipilimumab-nivolumab vs 43% for chemotherapy), and there was an intersection between the PFS curves of ipilimumab-nivolumab and chemotherapy with combinatorial immunotherapy gaining over time
“There was really no difference in median PFS. [The real difference] was in the duration of response (11 months for ipilimumab-nivolumab vs 6.7 months for chemotherapy),” Dr. Tsao said.
Dr. Tsao noted that immunotherapy, when offered alone, yields lower response rates in patients.
“What I think drives OS is the ability to maintain a response in patients who respond to immunotherapy,” she said. “When we compare all the trials, it appears that chemotherapy combined with immunotherapy has much higher response rates and drives the PFS benefit.”
She concluded by emphasizing the need to optimize treatment for patients, arguing that the most effective option will likely be the administration of chemotherapy and IO together.
“Combining chemotherapy and IO provides the best of both worlds. You have a higher response rate, and you still get OS and PFS benefits,” said Dr. Tsao. “The addition of pembrolizumab to pemetrexed and platinum improved OS with a 21% reduction in risk, improved PFS with a 20% reduction in risk, and increased the overall response rate. Therefore, it should be considered a new option for this patient population.”

Penelope Bradbury, MD, BCh, FACP, acknowledged the challenges of debating against the combination of chemotherapy with IO. Using humor, Dr. Bradbury recalled advice she received while preparing her counterargument. Among the experts she consulted were Quincy Chu, MD, FRCPm; Glenwood Goss, FCPSA, FRCPC; Natasha Leighl, BSc, MMSc, MD; and Frances Shepherd, MD, FRCPC.
Originally, Dr. Bradbury had planned to argue using cross-trial comparisons or highlighting median OS differences in IND227 and CheckMate 743, which Dr. Leighl described as “so last year.” Instead, Dr. Bradbury opted to pay heed to Dr. Goss’s advice to deflect and distract, which commenced a montage of slides ranging from adorable animals to a scenic Caribbean beach.
Ultimately, Dr. Bradbury took Dr. Shepherd’s advice to review the Kaplan-Meier curve for IND227 and ask whether Dr. Tsao could “drive a MAC truck through the curves.”
“In conclusion, my take-home message is even Dr. Anne Tsao cannot drive a MAC truck through the curves of IND227,” said Dr. Bradbury.
While the debate incorporated comedic elements, it also illuminated important insights into the potential of chemo-IO combinations. As Dr. Tsao demonstrated, the science data paint a clear benefit for chemotherapy with immunotherapy, with improved response rates, PFS, and OS illustrated from several key trials.
Additionally, the data show that those who undergo chemo-IO achieve initial tumor control and preserved DOR with IO maintenance, according to Dr. Tsao. Although research continues to evolve, these key insights may be a pivotal first step in helping patients with mesothelioma overcome the survival cliff.
Resources:
- 1. Bazhenova L, Kish J, Cai B, Caro N, Feinberg B. Real-world observational study of current treatment patterns and outcomes in recurrent or locally advanced/metastatic non-small cell lung cancer. Cancer Treat Res Commun. 2022;33:100637. doi:10.1016/j.ctarc.2022.100637