World Conference on Lung Cancer attendees received a sneak peek at the 9th Edition TNM Staging Classification during a special plenary session dedicated to the proposed updates.
Revisions to the global tumor, node, metastases (TNM) staging classification criteria for lung cancer, mesothelioma, and thymic cancer are in the final stages of preparation. The 9th Edition is set to be published jointly by IASLC, the Union for International Cancer Control, and the American Joint Committee on Cancer in early 2024.
The session took place on Monday, September 11, during WCLC 2023 in Singapore. The session can be viewed on-demand by registered attendees through December 31.
Setting the Stage

Hisao Asamura, MD, Chair of the IASLC Staging and Prognostic Factors Committee, began with an overview of the data used in preparing the 9th Edition guidelines. The period of diagnosis for the 2024 edition was 2011 to 2019. Data from more than 124,000 patients were submitted for consideration.
Among the 87,339 patients included in the analysis, 83% had non-small cell lung cancer (NSCLC) and 7% had small cell lung cancer (SCLC). For the first time, data from Asia/Australia represented a majority of responses at 56%. And Africa/Middle East made its debut in the lung cancer staging project with data from 172 patients (0.1%).
Dr. Asamura shared that the share of data collected via electronic data capture (EDC) rose to 25% with the new edition from 5% in the 8th edition, while batch data accounted for 75% of submissions.
This led session chair and then IASLC President-elect Paul Van Schil, MD, PhD, to encourage attendees to submit EDC data whenever possible: “This will strengthen the 10th edition even more because prospective data for EDC is much higher quality than retrospective batch data.”
Changes by Category—Lung Cancer
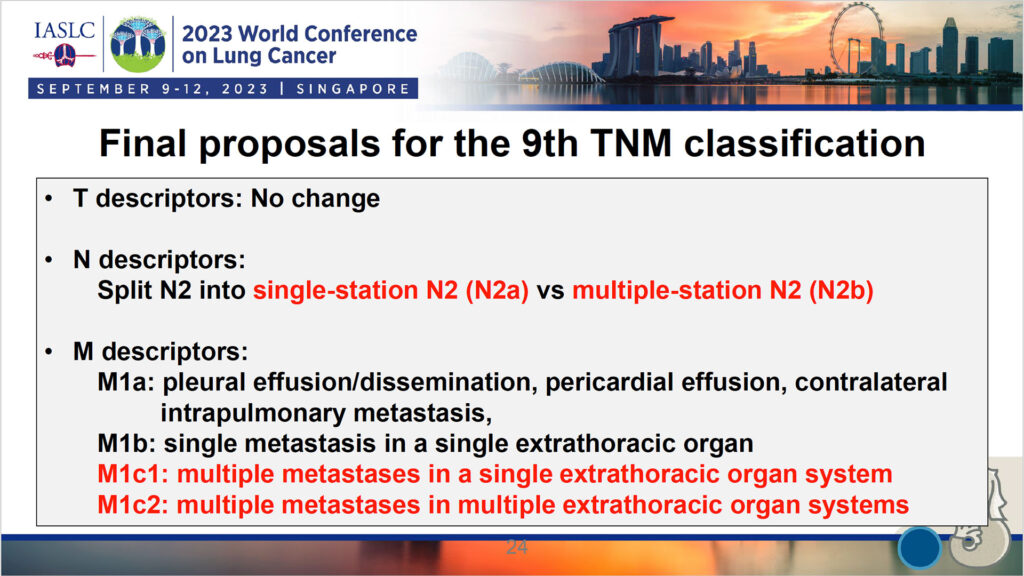
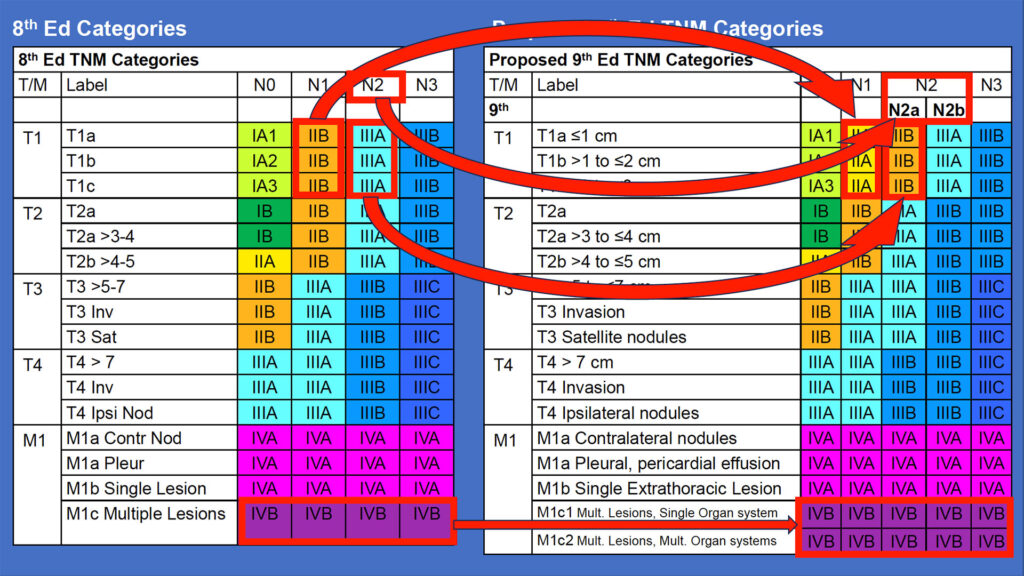
In summarizing the proposed changes to the lung cancer section of the 9th edition (see Figs. 1-2), Dr. Asamura noted that the group ultimately decided against making any changes to the T category. In analyzing T3, Chest Wall/PL3 was hypothesized to have worse survival than the other T3 descriptors, he said.
“Given inconsistent findings in clinical versus pathology results, the consensus was that there was insufficient evidence to change the Chest Wall/PL3 classification as a T3 descriptor,” Dr. Asamura explained.
In the N category, the previous N2 category will be split into two new subcategories: N2a and N2b. N2a will denote single-station N2 disease, while N2b will refer to multiple-station N2 disease.
Dr. Van Schil explained in answer to an attendee’s question that the concept of stations replaces the previous expectation of counting individual nodes.
“Lymph nodes often come out in pieces, so the pathologist often cannot count them precisely,” he said. “So we decided to talk about stations instead.”
The number of M1 subcategories will increase from four to five with the division of the previous M1c (multiple lesions) into two. M1c1 will denote multiple metastases in a single extrathoracic organ system and M1c2 will refer to multiple metastases in multiple extrathoracic organ systems.
Changes by Category—Mesothelioma

Next, Valerie Rusch, MD, FACS, Chair of the Pleural Mesothelioma (PM) Subcommittee, took the stage to discuss her group’s work. She began by providing the context that the group prioritized determining the importance of pleural thickness measurements.
“Simple three-level pleural thickness measurement is what’s realistic for clinicians around the world wherever CT imaging is available,” said Dr. Rusch, Attending Thoracic Surgeon, Vice Chair of Clinical Research, and Miner Family Chair of Intrathoracic Cancers at Memorial Sloan-Kettering Cancer in New York. “Our question was whether quantitative pleural thickness measurements should add to or replace existing qualitative T descriptors for clinical T staging.”
They concluded that both size (sum thickness) and extent of the primary tumor (involvement of anatomic structures) appear to be useful in constructing distinct T categories with respect to overall survival. Additionally, survival for patients with T1 with fissure involvement is similar to the 8th edition T2, she said.
“Nontransmural invasion of diaphragm (T2), lung parenchyma (T2), and endothoracic fascia (T3) cannot be accurately determined based on CT and should be removed as T descriptors,” Dr. Rausch said.
The group decided that no changes in N descriptors or categories from the 8th edition were necessary, Dr. Rausch said. For the M descriptors, the group reviewed additional data that support the 8th edition’s M0/M1 categories.
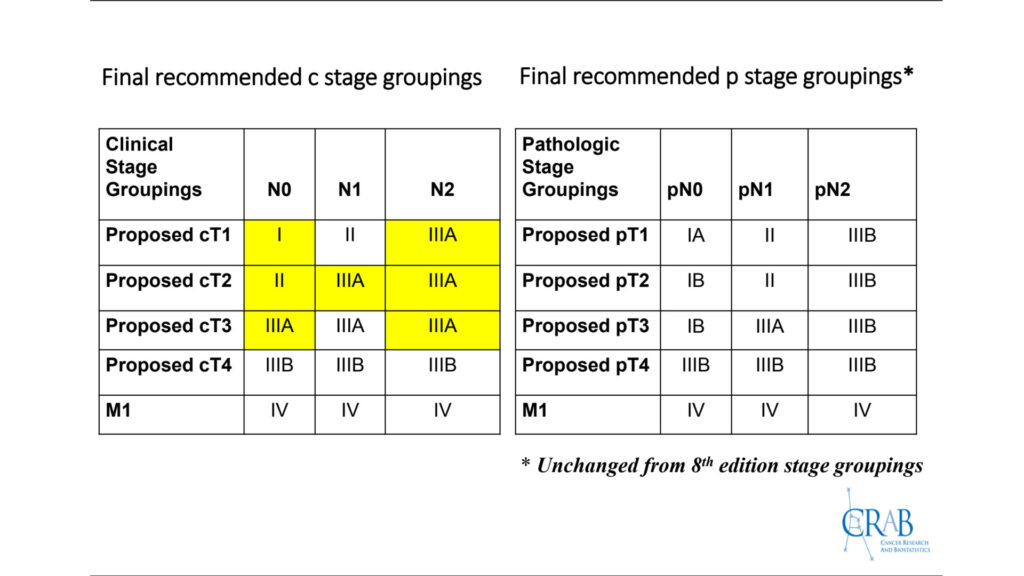
The changes in clinical T prompted adjustments to several clinical stage groupings, Dr. Rausch said. (See Fig. 3)
“In order to align with other cancer staging systems, metastatic disease M1 has been kept separate despite fairly close outcomes relative to stage IIIB. And the small numbers in the T1N1, T1N2, and T2N2 categories were assigned to stage groupings based on survival outcomes and committee consensus,” she explained. “The proposed groupings are statistically optimal but may be awkward for clinicians. We’re still in discussions, so stay tuned in that regard.”
Changes by Category—Thymic Tumors

Finally, Enrico Ruffini, MD, Chair of the Thymic Subcommittee, told attendees about his group’s recommendations, starting with methodological considerations. For this group of patients, the diagnosis period ranged from 1990 to 2021, which was appropriate for indolent tumors that require lengthy follow up, he said.
Of 9,000 patients included in the analysis, 62% came from Asia/Australia, Dr. Ruffini said. Only 4% of patients came from North America, down from 17% in the 8th edition.
The group considered relevant outcomes and determined that overall survival was more appropriate for late stages, while recurrence (including freedom from recurrence and cumulative incidence of recurrence) in R0 patients was more appropriate for early stages. The dataset contained batch data only (both retrospective and prospective), with no electronic data capture available.
The data were harmonized and merged into a central thymic database. “All analyses were done separately for thymoma, thymic carcinoma, and neuroendocrine tumors of the thymus,” Dr. Ruffini said. “But ultimately we arrived at one set of TNM recommendations for all thymic tumors, despite their different clinical behaviors.”
For the T descriptor, the group’s final proposals are to:
- Drop mediastinal pleura from the category.
- Subdivide T1 into T1a and T1b. T1a tumors will be 5 cm or less at the greatest dimension, while T1b tumors will be larger than 5 cm at the greatest dimension.
- Downstage T3 (lung) and T3 (phrenic nerve) to T2.
The group is recommending no changes to either the N descriptor or the M descriptor, Dr. Ruffini said.
The Staging and Prognostic Factors Committee includes 112 members. The committee is divided into four domains: lung cancer (which includes 14 subcommittees), thymic tumors, mesothelioma, and esophageal tumors. The anticipated publication list includes 28 papers to be published in 2023 and 2024 in the Journal of Thoracic Oncology.