Lung cancer is not only the leading cause of cancer deaths in the United States, with nearly 229,000 people diagnosed annually, but is also the deadliest cancer affecting patients of the Veterans Health Administration (VHA). More than 900,000 Veterans are at risk of developing lung cancer because of advanced age, environmental exposures, and/or smoking, according to VHA research.1
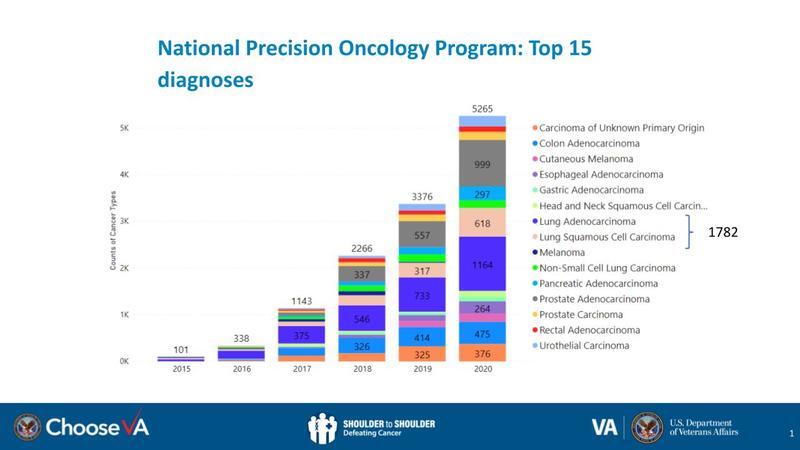
Each year, an estimated 7,700 Veterans who seek care in the VHA are diagnosed with lung cancer (Fig. 1).2
Currently, most are diagnosed at advanced stages, when survival is limited.
Fig 1. The 15 Most Common Diagnoses in the Veterans Health Administration National Precision Oncology Program (NPOP)
To better address care for this group of Veterans, VHA has established the Lung Precision Oncology Program (LPOP) to foster participation in lung cancer screening, genomic testing, and precision oncology trials with the goal of tailoring treatment to the needs of individual patients. The program is a component of the VHA’s Precision Oncology Initiative, which aims to transform VHA into a system of excellence in oncology care. LPOP is a joint effort between the U.S. Department of Veterans Affairs’ (VA’s) Office of Research and Development (ORD) and its National Oncology Program Office, with support from the Office of Healthcare Transformation. It provides resources to give VHA clinicians a range of tools and therapies to proactively address and treat lung cancer in Veterans (Fig. 2).
Fig. 2. Demonstration of Patient Receiving Low-Dose CT Scan to Screen for Lung Cancer
Says Dr. Sara Ahmed, director of Precision Oncology, VA National Precision Oncology Program, “Precision oncology means matching the right treatment to the right patient using a molecular understanding of their cancer. At the VA, we take it a step further—it’s an entire ecosystem of tools, resources, and systems of excellence across the United States that fosters personalized care for Veterans.”
Strategic Goals and Outreach
United States Veterans collectively share a unique set of risk factors that can affect their health for many years after military service. As a group, they are predominantly male and may have been exposed to a range of environmental hazards on military bases and during periods of deployment, such as burn pits and Agent Orange. They are more likely to be current or former smokers. They are also more likely to settle in rural areas of the country, where access to specialized oncology care is limited.
Through a competitive process that included peer review, the VHA established 20 hub sites to form a national learning network of VHA medical centers across the country for cutting-edge oncology care. There, LPOP will prioritize the implementation of low-dose chest CT scans for lung cancer screening to identify early-stage disease in Veterans at high risk, as well as smoking-cessation programs, genetic testing to improve access to precision-oncology clinical trials, and rapid translation of research discoveries into clinical care.
To reach Veterans where they live, irrespective of geography, management of hub sites is delegated to the regional Veterans Integrated Service Networks (VISNs). Each VISN will adopt a “hub and spoke” model to ensure that resources and clinical expertise are available to smaller healthcare facilities that may not support specialized cancer care but that care for an increasing number of rural or non-urban Veterans. To date, there are close to 80 VHA medical centers that are connected through the LPOP network (Fig. 3).
Fig. 3. Locations of the 20 VHA Medical Centers Comprising Hub Sites of the Lung Precision Oncology Program
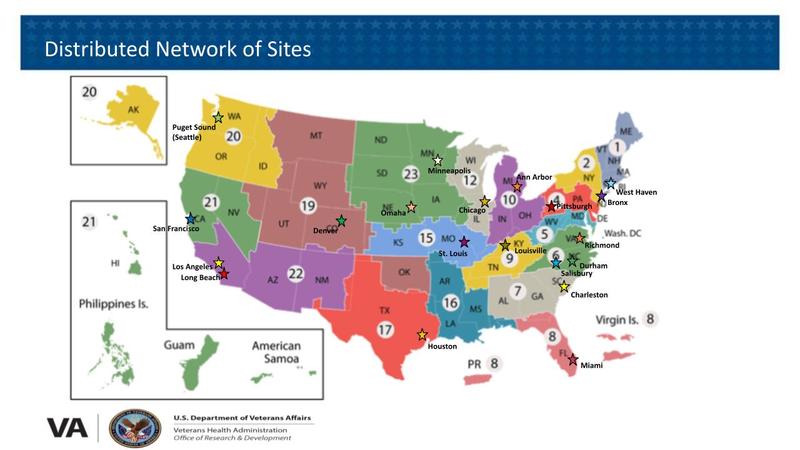
The 20 hub sites (Fig. 3) are located in Los Angeles, Long Beach, and San Francisco, California; Denver, Colorado; West Haven, Connecticut; Miami, Florida; Chicago, Illinois; Louisville, Kentucky; Ann Arbor, Michigan; Minneapolis, Minnesota; St. Louis, Missouri; Omaha, Nebraska; The Bronx, New York; Durham and Salisbury, North Carolina; Pittsburgh, Pennsylvania; Charleston, South Carolina; Houston, Texas; Richmond, Virginia; and Seattle, Washington.
In addition to LPOP’s primary focus on lung cancer screening and precision oncology trials, the VHA has set a number of goals to strengthen the program and increase Veterans’ access to services that allow the individualization of treatment options, specifically appropriate genomic testing and clinical trials that base eligibility on specific alterations identified in tumors. As a result, LPOP will enhance Veterans’ opportunities to benefit from a range of promising new treatment options for lung cancer, including novel and repurposed U.S. Food and Drug Administration—approved therapies.
The program will develop infrastructure to support research in precision oncology and lung cancer screening (e.g., development and assessment of new biomarkers and diagnostic tools) and to identify best practices for lung cancer care through research. To address improved disease detection, LPOP will expand lung cancer screening capabilities to monitor Veterans who are at risk for lung cancer and double the number of Veterans who are screened for lung cancer by 2022.
LPOP seeks to foster the development of early physician–scientists in lung cancer research, to leverage the VHA’s long-standing partnership with affiliated National Cancer Institute (NCI)–Designated Cancer Centers for their expertise, and to bring cutting-edge research and cancer care to Veterans. Of the 71 NCI-Designated Cancer Centers, 48 have academic affiliations or close geographic proximity to a VHA medical center.
The program will also make use of teleoncology services (Fig. 4) to increase access to care for Veterans who live long distances from the VHA facilities or for whom injury, illness, or other mobility issues make travel prohibitive. In Fiscal Year 2020, 162 Veterans with lung cancer received cancer care via teleoncology. The teleoncology program utilizes telehealth technologies such as VA Video Connect, which allows Veterans to virtually connect with their healthcare teams using computers or mobile devices, and will serve as a platform for future virtual clinical trials.
Fig. 4. A VHA Patient Meets with Dr. Michael Kelley via Teleoncology

Broadly, the VA’s ORD has made a commitment to expand access to cutting-edge clinical trials for Veterans in order to quickly bring research advances to the bedside. Toward that end, the VHA seeks engagement with Veterans and Veterans’ organizations and broad partnerships with academia, industry, federal agencies, philanthropic organizations, and professional societies to support LPOP’s research activities and accelerate the adoption of trial outcomes into the clinic.
Improving Outcomes for Veterans
Recently, the VA Preventive Medicine Field Advisory Committee adopted the updated U.S. Preventive Services Task Force (USPSTF) guidelines for lung cancer screening. The newer USPSTF guidelines recommend screening for people who are 50 to 80 years old, have a 20 pack-year smoking history, and are current or former smokers (within the last 15 years). The VHA encourages Veterans and their physicians to make joint decisions about screening after discussing its pros and cons. This balanced approach allows physicians and Veterans to learn from each other and will likely result in follow-through with screening and better outcomes for Veterans.
The rapid pace of change in precision oncology requires a learning healthcare system like VHA to be continually at the forefront of providing the highest quality of oncology care to Veterans. This is possible because clinical care and research at VHA work together so well. Precision medicine is a powerful tool that the VHA uses to improve oncology care for Veterans. To date, molecular testing of more than 20,000 samples from 126 VHA facilities has been completed through the VA National Precision Oncology Program (NPOP). The results from these tests have helped to guide treatment decisions, many based on genetic alterations identified in patients’ tumors (Fig. 5). Clinicians are provided an opportunity to access expert advice through on-demand electronic consultation or discuss difficult cases with experts on the molecular oncology tumor board (MOTB). In the case of treatment-resistant tumors, this type of expert consultation with the MOTB can facilitate individualized therapy that can mean the difference between life and death.
Creating and Running LPOP
LPOP builds on work that was initiated in partnership with the Cancer Moonshot, an initiative spearheaded by then–Vice President Joe Biden. In 2016, those early efforts led to the establishment of the NPOP, which provides clinical-grade, tumor-gene molecular panel testing and consultative services for treating Veterans with cancer.3
The Precision Oncology Initiative was catalyzed by a $50 million commitment from the Prostate Cancer Foundation to establish the Precision Oncology Program for Cancer of the Prostate. This was followed by strategic investments by VHA leadership in Fiscal Year 2021 to establish LPOP.
Similarly, the foundations for lung cancer screening were laid with the VHA Lung Cancer Screening Demonstration Project, created to establish the feasibility of conducting low-dose chest CT testing1
after the strategy was shown in 2011 to be effective for identifying disease in patients at high risk of developing lung cancer.4
This was followed by partnerships with various organizations, including funding from the Bristol Myers Squibb Foundation, to create the VHA Partnership to Increase Access to Lung Screening; this effort focused on reducing lung cancer mortality for Veterans through increased access to low-dose CT screening. As a result, VHA established itself as a champion of early lung cancer screening for Veterans.
Fig. 5. Driver Mutations and Treatment Recommendations Based on the Results of Next-Generation Sequencing of NSCLC Specimens
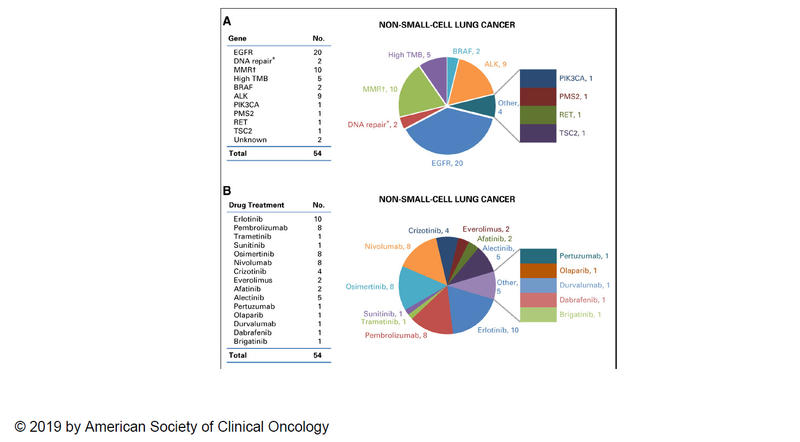
A: Distribution of actionable mutations (i.e., eligible for on- or off-label use of a U.S. Food and Drug Administration–approved targeted therapy or immune checkpoint inhibitor on the basis of NGS test results). B: Targeted and immunotherapy drugs prescribed after NGS testing. Data are reported as the name of gene or drug (no.; number). Reprinted from Poonnen.5
Abbreviations: MSI-H, microsatellite instability-high; TMB, tumor mutational burden. *DNA repair genes (e.g., BRCA1, BRCA2, ATM, ATR). †Mismatch repair (MMR) genes (e.g., MLH1, MSH2, MSH6, PMS2).
LPOP is governed by an executive steering committee co-chaired by the VA national program director for oncology and ORD’s chief research and development officer, with coordination provided by the Cooperative Studies Program (CSP) Coordinating Center at the West Haven VA Medical Center in Connecticut. The executive steering committee is assisted by program staff from the National Oncology Program Office, ORD, the Office of Healthcare Transformation, and the CSP Coordinating Center to facilitate LPOP operation, and provides opportunities within the network for investigators to develop and demonstrate leadership in areas that are suited to their particular interests.
- 1. a. b. Kinsinger LS, Anderson C, Kim J, et al. Implementation of Lung Cancer Screening in the Veterans Health Administration. JAMA Intern Med. 2017;177(3):399-340.
- 2. Williams, CD, Moghanaki, D. Lung Cancer in the VA at a National Level. Federal Practitioner. (theme issue: 2019 Cancer Data Trends)
- 3. Kelley, MJ. VA National Precision Oncology Program. Fed Pract. 2020;37(suppl 4):S22-S27.
- 4. National Lung Screening Trial Research Team; Aberle DR, Adams AM, et al. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med. 2011;365(5):395-409.
- 5. Poonnen PJ, Duffy JE, Hintze B, et al. Genomic Analysis of Metastatic Solid Tumors in Veterans: Findings From the VHA National Precision Oncology Program. JCO Precis Oncol. eCollection 2019.