The COVID-19 pandemic has undoubtedly altered patient care as countries have locked down to prevent spread of the virus and shifted resources to accommodate surging caseloads. It has also taken a considerable emotional toll on vulnerable individuals, particularly patients with cancer, given fears about contracting the virus and concerns about disruptions in care.
Several researchers presented enlightening data at the 2020 World Conference on Lung Cancer documenting trends in how the pandemic has influenced lung cancer healthcare delivery over the past year and the consequences on patients’ physical and emotional health.
Influence of the Pandemic on Lung Cancer Diagnosis and Prognosis
Roxana Reyes, MD, of the Hospital Clinic of Barcelona, presented findings from a descriptive study in Spain suggesting that the COVID-19 pandemic has led to fewer diagnosed cases of lung cancer but more symptomatic disease among those diagnosed, in turn leading to poorer patient outcomes (Abstract MA03.08).
As she explained, the first wave of COVID-19 infection in Spain was particularly devastating, lasting from March to June 2020. As the number of infections and deaths shot up during this period, drastic healthcare changes ensued.
“A state of emergency forced the prioritization of health services, which could delay the diagnosis and cancer treatment,” Dr. Reyes said.
To understand how these changes influenced lung cancer diagnosis, severity, and clinical outcomes, Dr. Reyes and colleagues compared retrospective data from two tertiary hospitals in Spain over the same January-to-June time period in 2019—pre-COVID—and in 2020—during COVID.
Of the 162 individuals with newly diagnosed lung cancer included in the study, the rate of diagnosis fell by 38% during the COVID period relative to the pre-COVID period. Reductions in new diagnoses were fairly consistent for the two major histologic subtypes. NSCLC diagnoses fell from 67 cases during the pre-COVID period to 43 cases during the COVID period—a decrease of 36%. SCLC diagnoses fell from 33 cases during the pre-COVID period to 19 cases during the COVID period—a decrease of 42%.
Notably, patients diagnosed with lung cancer during the COVID timeframe were more likely to be symptomatic than their pre-COVID counterparts.
Respiratory symptoms were more common at diagnosis among patients with NSCLC during the COVID period versus the pre-COVID period (30% vs. 23%). Consistent with this observation, locally advanced or advanced disease was also more common among patients diagnosed during the COVID period versus the pre-COVID period (81% vs. 69%). Although a similar proportion of newly diagnosed cases required hospitalization during COVID versus pre-COVID (21% vs. 18%), in-hospital mortality was markedly higher for patients diagnosed during COVID versus before COVID (44% vs. 17%).
These results were not as dire for patients with SCLC. Although respiratory symptoms were more common among patients diagnosed with SCLC during COVID versus pre-COVID (32% vs. 24%), outcomes were no poorer for the COVID cohort with regard to disease stage, hospitalizations, or death during hospitalization.
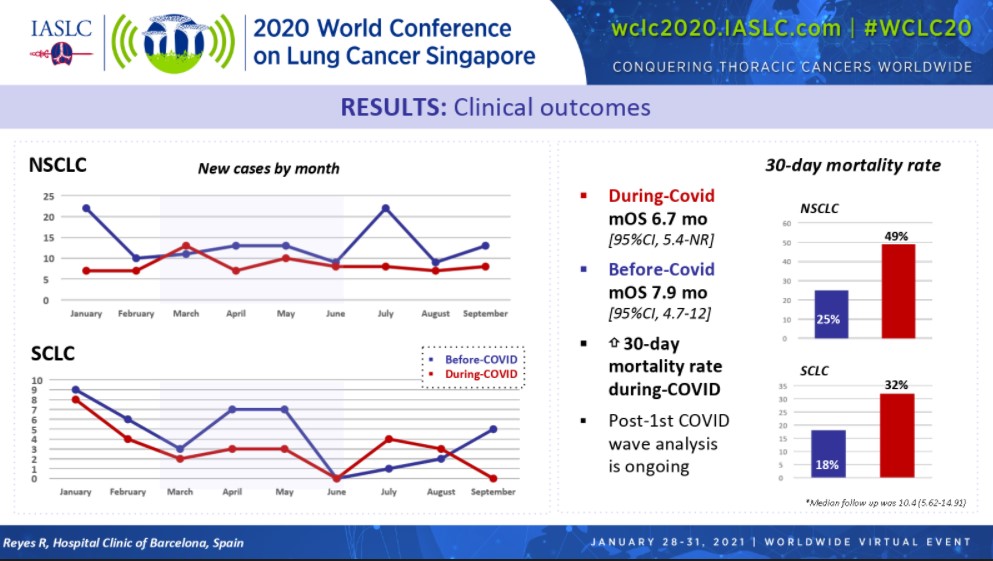
Some of the most interesting data Dr. Reyes presented pertained to patient survival. In the overall group of patients with lung cancer, median overall survival reached 7.9 months for the pre-COVID cohort compared with 6.7 months for the COVID cohort (Figure). In line with these findings, 30-day mortality rates for the pre-COVID and COVID groups were 25% and 49%, respectively, for patients with NSCLC, and 18% and 32%, respectively, for patients with SCLC.
“There is a mortality rate which almost doubled during COVID in comparison with 2019 in both histologies,” Dr. Reyes stated.
“Some of the limitations of this study include small sample size, the retrospective nature of the study, and no statistics or P values,” noted Jay M. Lee, of the Ronald Reagan UCLA Medical Center in Los Angeles, in his review of these data.
To provide better context for the Spanish findings, Dr. Lee showed recently published data from a similar but larger retrospective study conducted in Korea evaluating COVID-19 effects.1 In this analysis, the number of incident lung cancer diagnoses remained consistent across the pre-COVID and COVID periods, unlike Dr. Reyes’ data. However, similar to Dr. Reyes’ findings, the Korea study documented a significant increase in the diagnosis of late-stage disease in tandem with a reduction in early-stage disease, suggesting delayed diagnosis.
“The COVID-19 pandemic is likely to last for a prolonged period of time, and we have to make a special effort for ensuring the cancer diagnosis and clinical care of our patients,” Dr. Reyes emphasized.
This session had a real-time Q&A that provided attendees with the opportunity to ask questions of the session participants. The Q&As are included in the On-Demand recordings, available through the virtual platform. Registration is ongoing for the next 90 days at wclc2020.iaslc.org.
Other COVID-19 Research Spanning Diagnostics to Patient Advocacy
Radiotherapy Simulation CT for COVID-19 Screening
Given the rapidity at which the COVID-19 pandemic set in, healthcare providers have sometimes devised creative solutions to rein in the virus. Toward this end, researchers at the Memorial Sloan Kettering Cancer Center in New York, a pandemic epicenter at the start of the outbreak, sought to determine whether radiotherapy-associated CT imaging could be used to screen asymptomatic individuals for COVID-19 infection (Abstract P02.14).
Unfortunately, their idea did not succeed. Of 400 patients who underwent CT simulation scanning of the lungs prior to radiotherapy, 17% had findings suspicious for COVID-19 when reviewed by radiation oncologists according to consensus criteria. However, only a handful of these individuals (3 of 23 with available COVID test results) were actually infected with COVID-19 based on PCR testing. Given the lack of correlation between radiographically suspicious simulation CT scans and COVID-19 positivity, as well as discordance between radiation oncologists and diagnostic radiologists in classifying scans as suspicious, the investigators concluded that “these results suggest that routine review of radiotherapy simulation CT scans is of limited value in identifying asymptomatic COVID-19 infection.”
Analysis of Outcomes in Patients With Thoracic Malignancies and COVID-19 Infection by Ethnicity and Gender
The COVID-19 pandemic has shined a stark light on healthcare disparities among various populations. Emerging data from TERAVOLT, a multicenter, international, observational study designed to help track outcomes in patients with thoracic cancer and a confirmed COVID-19 diagnosis, help to document some of these imbalances (Abstract P09.18).
As of August 2020, 1,053 patients from 19 countries had been included in the TERAVOLT registry, including 84% Whites, 9.3% Blacks, and 25% Hispanics. An analysis of clinical outcomes by ethnicity showed that although similar proportions of whites, blacks, and Hispanics were hospitalized for COVID-19 infection, mortality rates were highest for Hispanics (36%) and whites (34%), as compared with blacks (26%).
Analysis of outcomes by gender showed that despite similar performance status scores between men and women, men were more likely than women to be admitted to the hospital (77% vs. 66%) and more likely to die in the hospital (37% vs. 28%).
Virtual Prehabilitation for Patients Scheduled for Lung Cancer Surgery
Patients slated for lung cancer surgery who receive prehabilitation demonstrate reductions in postoperative complications, morbidity, and hospital length of stay following the operation. Unfortunately, the COVID-19 pandemic has hampered patients’ ability to participate in face-to-face prehabilitation exercise programs due to the need for social distancing.
Providers at a busy National Health Service Trust in London developed a virtual prehabilitation service for patients undergoing lung surgery. They captured results showing that the virtual program is both feasible and effective at improving patients’ presurgical physical activity levels and exercise capacity (Abstract OA08.04).
Patient Support—Understanding the Needs and Rising to the Challenge
In June 2020, the LUNGevity Foundation conducted a survey of US patients with lung cancer and their caregivers to identify patient needs amidst the COVID-19 pandemic (Abstract MA07.08). The 302 respondents who completed the survey, one-third of whom lived in COVID-19 hotspots, indicated the following:
- 46% reported interruptions in lung cancer care—a problem cited by more younger patients than older patients (≤ 65 vs > 65 years old; 53% vs 34%).
- 96% were concerned that the pandemic would affect their cancer care, especially patients living in COVID-19 hotspots (99% of these individuals reported this as a concern).
- 45% worried about accessing care even after shelter-in-place restrictions were lifted.
- Only about half of the respondents had spoken with their doctors about these concerns.
Aligned with these findings, three studies from around the globe documented increased levels of psychological distress associated with the COVID-19 pandemic among patients with lung cancer.
- A study in Italy conducted in outpatients with lung cancer, lymphoma, or breast cancer found that 54% of individuals had above-normal levels of anxiety and depression, and 23% met the criteria for severe levels of posttraumatic stress disorder (Abstract FP06.04). Importantly, patients with lung cancer reported significantly higher levels of stress and anxiety compared with patients with lymphoma or breast cancer.
- In a survey conducted in Japan, roughly half of the patients with lung cancer receiving treatment felt anxious about being exposed to the virus (Abstract MA07.09). Notably, these rates were even higher among patients not under treatment.
- Patients with lung cancer in Canada reported increased levels of anxiety, particularly surrounding the ability to spend time with loved ones and participate in life events (Abstract P38.08). To help alleviate their anxiety, they desired clear communication from their healthcare team, along with increased communication from lung cancer organizations.
These findings underscore the need for psychosocial support for patients with lung cancer during these trying times. Although lung cancer organizations are rising to the challenge to buoy patients’ mental well-being, they, too, are being adversely affected by the COVID-19 pandemic.
The Global Lung Cancer Coalition, a partnership of 40 patient organizations across 29 countries, conducted a survey of its members between April and May of 2020 to gauge the effects of COVID-19 on the organizations’ ability to support patients (Abstract MA07.07). Of the 22 organizations that responded to the survey, 64% reported receiving more requests from patients since the start of the pandemic through a variety of channels, including calls to telephone helplines, email requests, and requests via Facebook and their websites. Whereas 67% of responding organizations had to close some patient services (primarily face-to-face activities), 86% introduced new digital or no-contact services to help address patient needs (eg, online consultations, extending helpline hours, providing more web content and podcasts). Yet despite providing more support to patients during the pandemic, 67% of responding organizations reported decreases in their funding, 45% worried about being able to continue to employ staff, 35% worried about being able to provide the same level of patient services, and 25% worried about their survival.
“Patient organizations need urgent support to continue to meet increased patient needs, and for some to survive,” the Global Lung Cancer Coalition research team concluded.
Reference
- Park JY, Lee YJ, Kim T, et al. Collateral effects of the coronavirus disease 2019 pandemic on lung cancer diagnosis in Korea. BMC Cancer. 2020;20(1):1040.