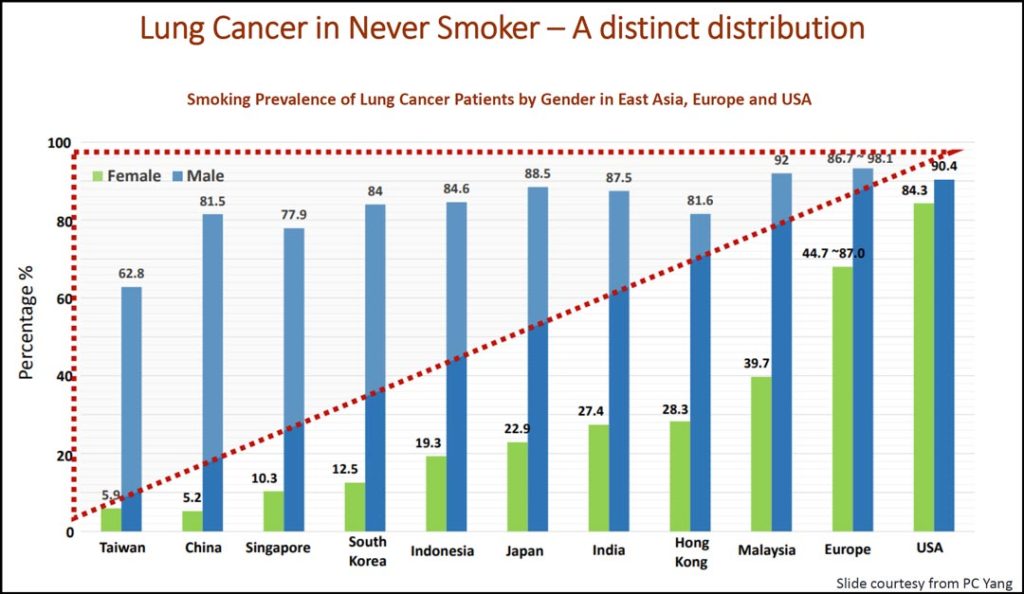
Lung cancer in patients who have never smoked is a global rising threat, especially in East Asia, where in such countries as Taiwan, China, and Singapore you see low prevalence (<10%) of smokers among female lung cancer patients (Table 1).
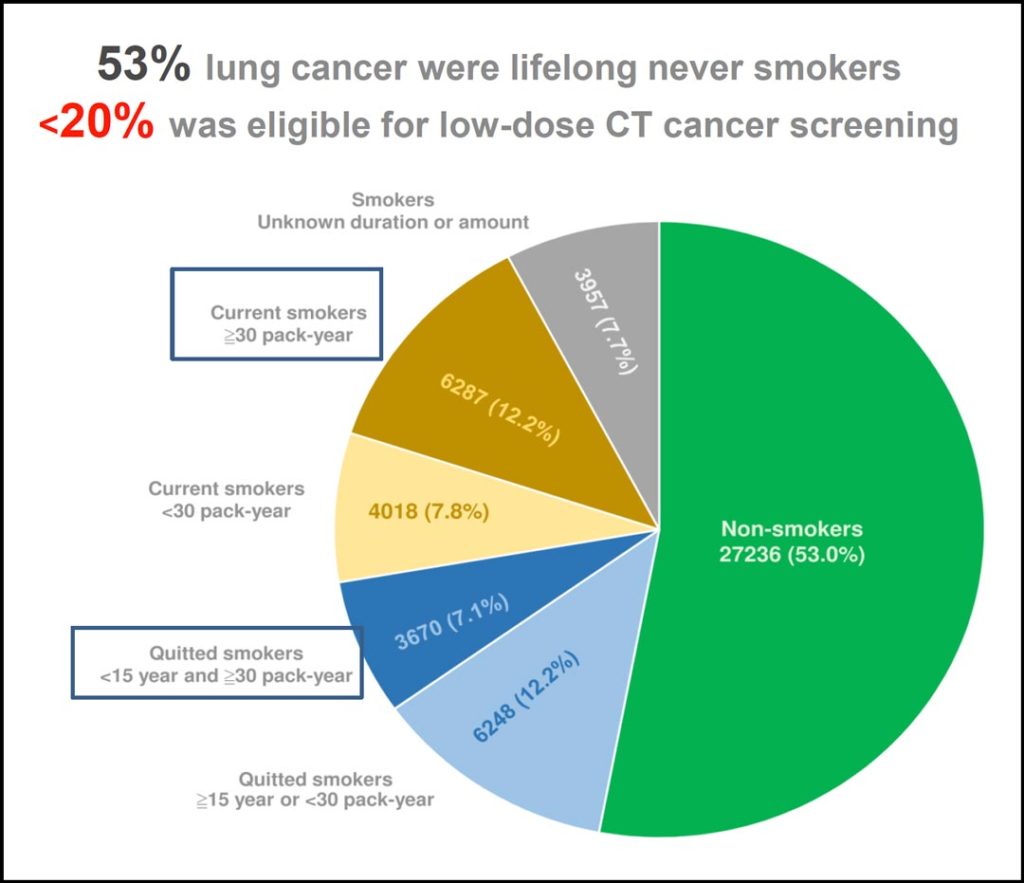
So said Gee-Chen Chang MD, PhD, during a lecture at the 2022 Asia Conference on Lung Cancer. Indeed, Dr. Chang, who is with the division of pulmonary medicine in the department of internal medicine and Chung Shan Medical University Hospital in Taichung, Taiwan, said a study of nearly 58,000 lung cancer cases in Taiwan showed more than 50% of patients had never smoked. (Table 2)
Dr. Chang said there are many problems to be solved when it comes to improving detection of lung cancer in patients who never smoked:
- Current screening guidelines and eligibility criteria can miss more than 30% to 50%, even in smokers.
- A strategy for reducing lung cancer mortality is needed to identify high-risk non-smokers and offer them (LDCT) screening.
- Developing such a strategy requires assembling risk factors into a risk prediction model.
“We need a different strategy for lung cancer screening,” he said. “We know from NLST and NELSON that LDCT screening has a mortality benefit in lung cancer. One major benefit is stage shift to early-stage disease. However, randomized lung cancer screening trials all looked at smokers. From our previous study, we know less than 20% of our lung cancer patients were eligible for LDCT cancer screening based on NLST study criteria.” (Table 2)
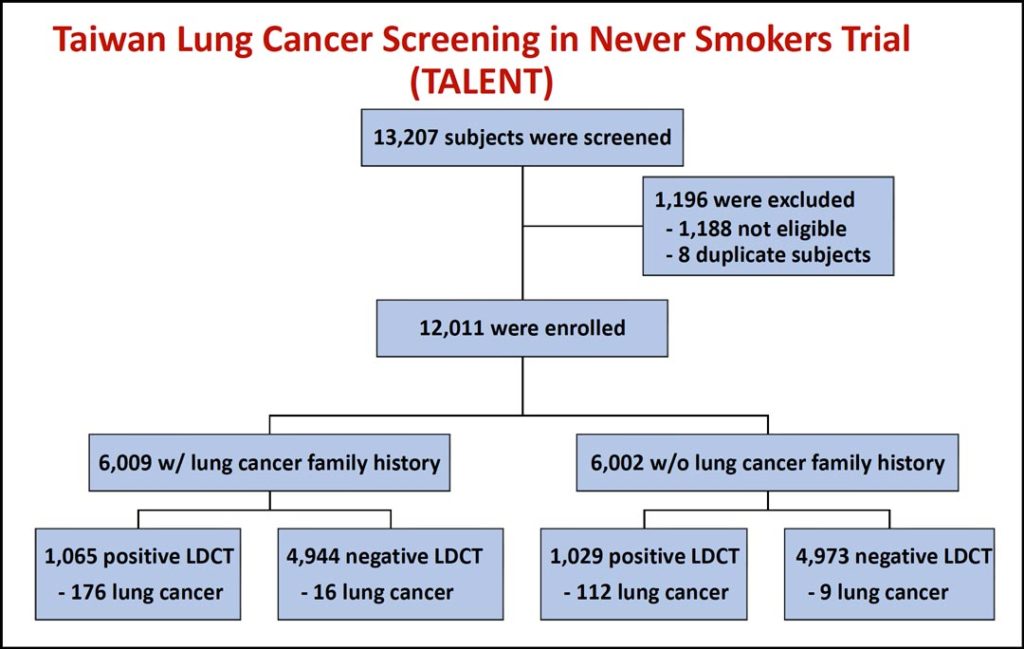
While developing an accurate risk predication model for patients who have never smoked will be challenging, researchers have made progress as demonstrated in the TALENT (Taiwan Lung Cancer Screening for Never Smoker Trial) study, which Dr. Chang reviewed during his lecture.
TALENT used a nationwide LDCT lung cancer screening campaign for this population. Although participants had never smoked, they did to have one or more of the following risks:
- Family history of lung cancer within the third-degree
- Passive smoking exposure
- Tuberculosis or chronic obstructive pulmonary disease
- Cooking index score ≥ 110 (measured by number of times per week cooking included pan-frying, stir-frying, or deep-frying multiplied by number of years spent cooking)
- Cooking without ventilation
A total of 12,011 subjects were enrolled. Half the participants had a family history of lung cancer. (Table 3)
“We found that family history of lung cancer may increase the risk of lung cancer,” Dr. Chang said. “The prevalence of lung cancer was 3.3% and 2.0% in subjects with and without lung cancer family history, respectively. The TALENT study shows that LDCT screening of people who have never smoked but who have other risk factors may result in a beneficial stage-shift for this population.”

Dr. Chang highlighted other key findings from TALENT as well.
- TALENT T0 lung cancer detection was 2.6%—higher than NLST (1.1%) and NELSON (0.9)
- Lung cancer detected in TALENT T0: 96.5% stage 0-1
- A potential risk prediction model for lung cancer in patients who never smoked was generated
- LDCT lung cancer screening in high-risk patients who never smoked may be feasible
“Lung cancer in non-smokers is a global rising threat, especially in East Asia,” Dr. Chang said. “A risk prediction model is needed for screening this high-risk population—assembling risk factors, including data on air pollution and other carcinogens. Finally, useful biomarkers identified in non-smokers at high risk for lung cancer may be needed. Combining biomarkers with an accurate risk prediction model may improve the clinical use.”