The COVID-19 pandemic has caused more than 43.2 million cumulative cases and 1.16 million deaths, as of late October 2020. Approximately 1% of patients with COVID-19 have malignancy,1 and lung cancer accounts for a considerable portion of these malignancies. Patients with lung cancer have often experienced severe disease when they contract COVID-19,2 which highlights the importance of accurate and prompt diagnosis of COVID-19 in lung cancer management. Although the reference diagnostic for COVID-19 is a reverse transcription polymerase chain reaction, COVID-19 can be incidentally detected on a chest CT scan, which is a salient imaging modality for diagnosis and monitoring of lung cancer.
Chest CT Findings of COVID-19
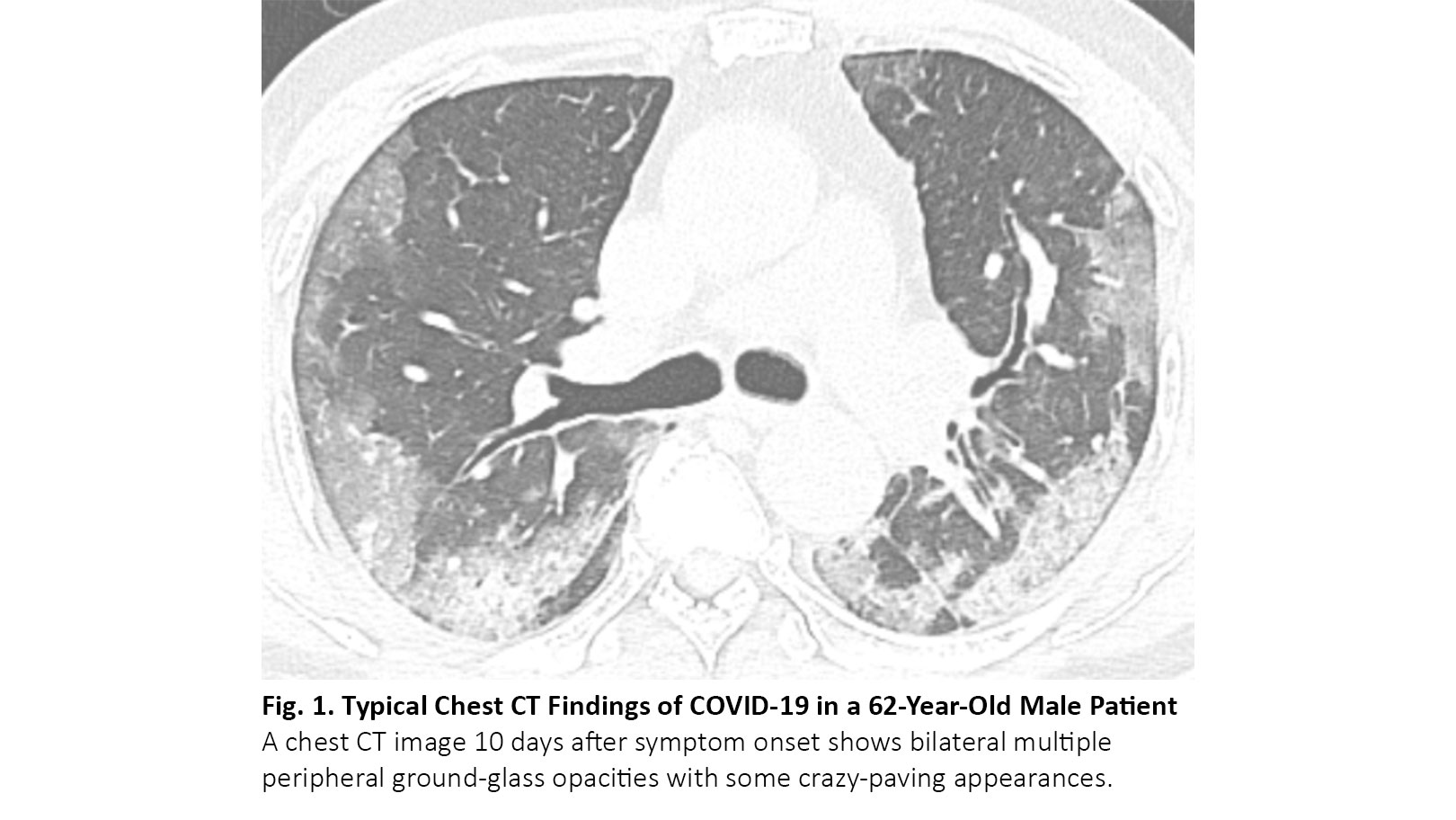
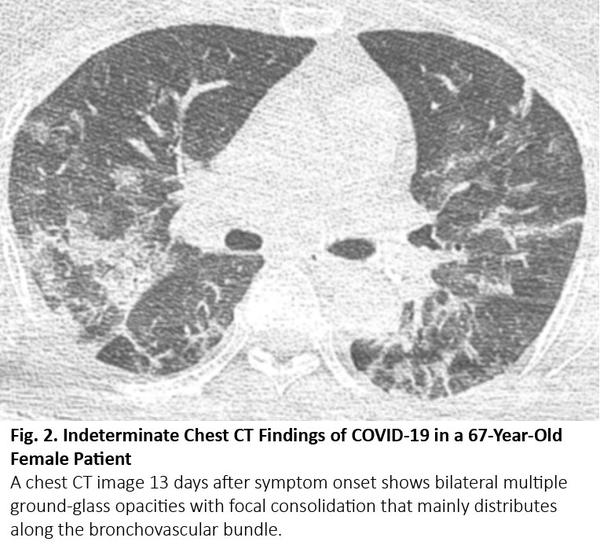
COVID-19 typically manifests as bilateral, multiple ground-glass opacities with a predilection for the lung periphery on chest CT images3 (Fig. 1). Between 61% and 72% of patients with COVID-19 had the typical CT findings around 1 week after symptom onset, whereas fewer than 10% of non–COVID-19 patients had these findings.4,5 COVID-19 may accompany focal consolidation and reticular opacities (crazy-paving appearance) or other findings of organizing pneumonia, such as reversed halo sign. Between 17% and 20% of patients with COVID-19 had nonspecific CT findings indistinguishable from various infectious and noninfectious diseases such as hypersensitivity pneumonitis, pneumocystis pneumonia, and diffuse alveolar hemorrhage (Fig. 2). Between 3% and 17% of patients with COVID-19 had CT features atypical for COVID-19 infection. A considerable portion of patients with COVID-19 can have a CT scan that is negative for abnormalities; these negative CT results are more frequently found in children and asymptomatic patients without comorbidities.6 The timing of CT scanning after symptom onset also affects the recognition and degree of CT abnormalities. Up to 56% of patients with COVID-19 can have a normal CT scan within 2 days of symptom onset,7 and the degree of CT abnormalities increases as symptoms last, peaking around 10 days after symptom onset.8
Chest CT imaging provides a sensitivity of 93% and specificity of 37% for COVID-19, on average.6 With additional cases of COVID-19 accumulating, one study reported an improved specificity of chest CT around 80%, while sensitivity remained above 90%.9
Infectious and Noninfectious Diseases With CT Findings Similar to COVID-19
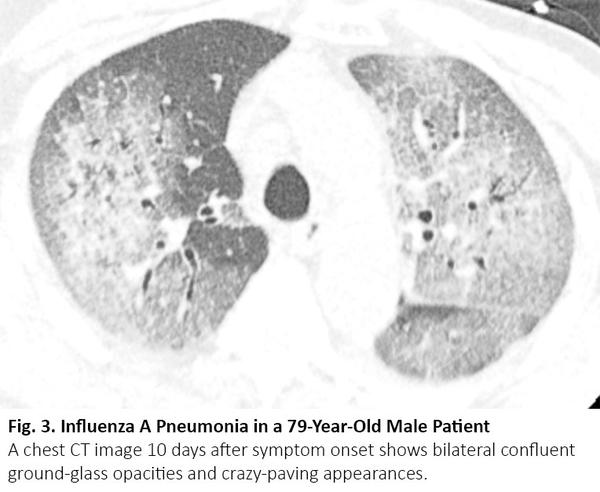
Patients with lung cancer may have CT abnormalities similar to those of COVID-19 during the course of the disease, but due to other reasons, such as viral pneumonia caused by treatment-induced pneumonitis, cancer recurrence, and interstitial lung disease. Viral pneumonia, especially influenza pneumonia, can manifest as bilateral ground-glass opacities and consolidation with similar geographic distributions on chest CT images10 (Fig. 3). The radiologic differentiation can be problematic in the fall and winter, when influenza prevails. Nevertheless, interlobular septal thickening and round opacities with the typical peripheral distribution were more frequent in COVID-19 pneumonia than influenza pneumonia, whereas nodules and tree-in-bud sign were less frequent in COVID-19.11
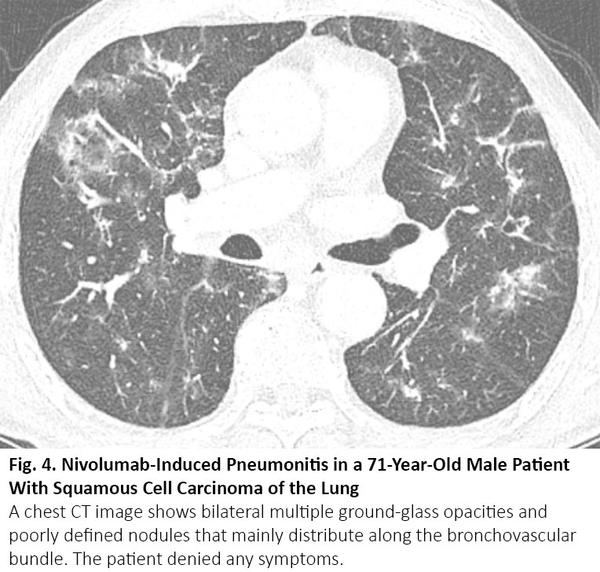
Chemotherapy or immunotherapy can cause drug-induced pneumonitis that manifests as various radiologic patterns of interstitial lung disease.12 The most frequent pattern is cryptogenic organizing pneumonia, followed by nonspecific interstitial pneumonia, hypersensitivity pneumonitis, and acute interstitial pneumonia.13 Among them, cryptogenic organizing pneumonia or nonspecific interstitial pneumonia pattern can radiologically mimic COVID-19 pneumonia (Fig. 4), and vice versa.14
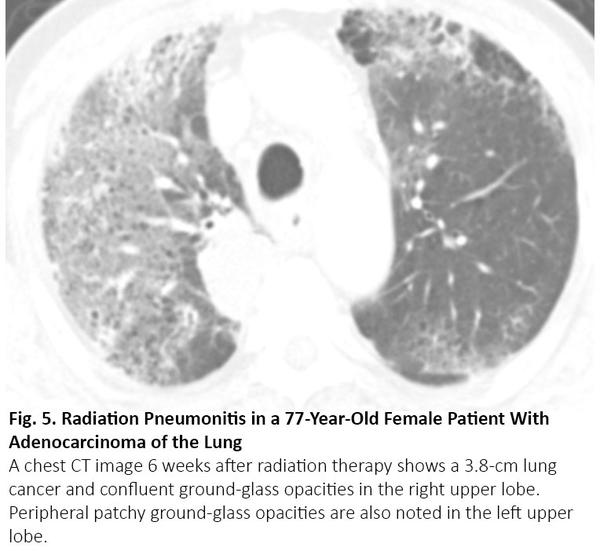
Radiation pneumonitis occurs within 4 to 12 weeks after completion of radiation, sometimes later.15 Because radiation pneumonitis usually occurs within the irradiated lung as a localized form, radiation pneumonitis outside the treatment portal is unusual. Therefore, radiologic differentiation from COVID-19 pneumonia can be straightforward in most cases. Nevertheless, radiation pneumonitis may be indistinguishable from COVID-19 pneumonia when the pneumonitis distributes diffusely (Fig. 5).
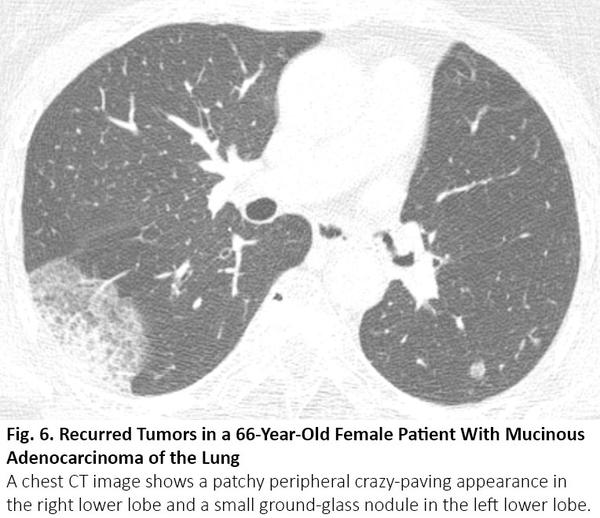
Lung cancer usually manifests as a nodule or mass, but sometimes it can show an airspace pattern. Invasive mucinous adenocarcinoma is a well-known example that can be seen as consolidation with or without ground-glass opacity, mimicking pneumonia. Adenocarcinoma with particular subtypes, including lepidic, acinar, and papillary-predominant subtypes, can be seen as areas of ground-glass opacity on CT.16 When these lesions exist in multiple sites in the lung, chest CT images may share similar radiologic findings with COVID-19 (Fig. 6). The persistence of these lesions on previous CT can provide a solution for the differentiation.
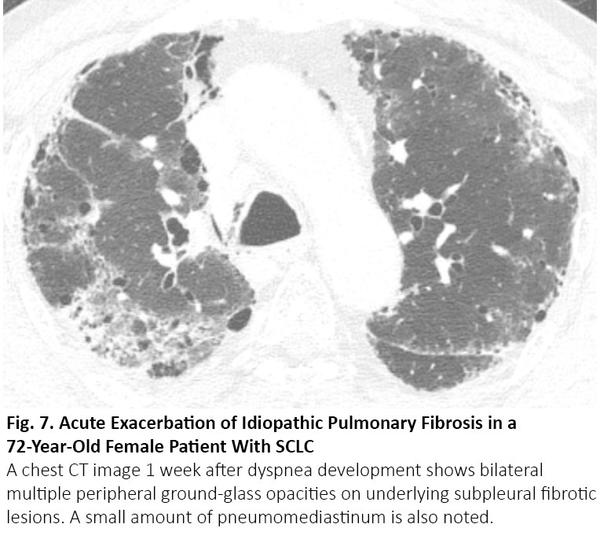
Because smokers are at risk for both lung cancer and idiopathic pulmonary fibrosis, lung cancer frequently occurs in patients with idiopathic pulmonary fibrosis. When patients undergo surgery or radiation therapy, acute exacerbation of idiopathic pulmonary fibrosis can be seen as bilateral diffuse or peripheral ground-glass opacity in the lung,17 as with COVID-19 pneumonia (Fig. 7).
In conclusion, COVID-19 pneumonia can cause deterioration in patients with lung cancer, and it shares chest CT abnormalities that can be seen during the management of lung cancer. It may not be easy to differentiate COVID-19 pneumonia and non−COVID-19 diseases solely on the basis of chest CT images. Physicians should cautiously treat patients with lung cancer and ground-glass opacities on chest CT images, while assessing the probability of COVID-19 pneumonia and applying reverse transcription polymerase chain reaction testing to confirm or refute COVID-19 infection.
References:
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335-337.
- Luo J, Rizvi H, Preeshagul IR, et al. COVID-19 in patients with lung cancer. Ann Oncol. 2020. [Epub ahead of print].
- Simpson S, Kay FU, Abbara S, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology: Cardiothoracic Imaging. 2020;2(2):e200152.
- Ciccarese F, Coppola F, Spinelli D, et al. Diagnostic accuracy of North America Expert Consensus Statement on Reporting CT Findings in Patients with Suspected COVID-19 Infection: an Italian single center experience. Radiology: Cardiothoracic Imaging. 2020;2(4):e200312.
- Prokop M, van Everdingen W, van Rees Vellinga T, et al.. CO-RADS: a categorical CT assessment scheme for patients suspected of having COVID-19 – definition and evaluation. Radiology. 2020;296(2):E97-E104.
- Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020. [Epub ahead of print].
- Bernheim A, Mei X, Huang M, et al. Chest CT findings in Coronavirus Disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):200463.
- Pan F, Ye T, Sun P, et al. Time course of lung changes at chest CT during recovery from Coronavirus Disease 2019 (COVID-19). 2020;295(3):715-721.
- Falaschi Z, Danna PSC, Arioli R, et al. Chest CT accuracy in diagnosing COVID-19 during the peak of the Italian epidemic: a retrospective correlation with RT-PCR testing and analysis of discordant cases. Eur J Radiology. 2020. [Epub ahead of print].
- Agarwal PP, Cinti S, Kazerooni EA. Chest radiographic and CT findings in novel swine-origin influenza A (H1N1) virus (S-OIV) infection. Am J Roentgenology. 2009;193(6):1488-1493.
- Liu M, Zeng W, Wen Y, Zheng Y, Lv F, Xiao K. COVID-19 pneumonia: CT findings of 122 patients and differentiation from influenza pneumonia. Eur Radiol. 2020. [Epub ahead of print].
- Ryu JH. Chemotherapy-induced pulmonary toxicity in lung cancer patients. J Thorac Oncol. 2010;5(9):1313-1314.
- Nishino M, Ramaiya NH, Awad MM, et al. PD-1 inhibitor-related pneumonitis in advanced cancer patients: radiographic patterns and clinical course. Clin Cancer Res. 2016;22(24):6051-6060.
- Artigas C, Lemort M, Mestrez F, Gil T, Flamen P. COVID-19 pneumonia mimicking immunotherapy-induced pneumonitis on 18F-FDG PET/CT in a patient under treatment with nivolumab. Clin Nucl Med. 2020;45(8):e381-e382.
- 15. Choi YW, Munden RF, Erasmus JJ, et al. Effects of radiation therapy on the lung: radiologic appearances and differential diagnosis. Radiographics. 2004;24(4):985-997, 998.
- Austin JH, Garg K, Aberle D, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013;266(1):62-71.
- Kim DS, Park JH, Park BK, Lee JS, Nicholson AG, Colby T. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur Respir J. 2006;27(1):143-150.