According to an updated analysis of the IASLC’s 2014 prognostic factors for pleural mesothelioma presented at the 2023 World Conference on Lung Cancer, data support and improve upon the existing model; they also underscore the importance of systematically collecting updated biomarker data to improve prognostic value. The original 1995-2009 database of 3,101 patients was validated with an updated cohort of 1,733 patients from 2009-2019.

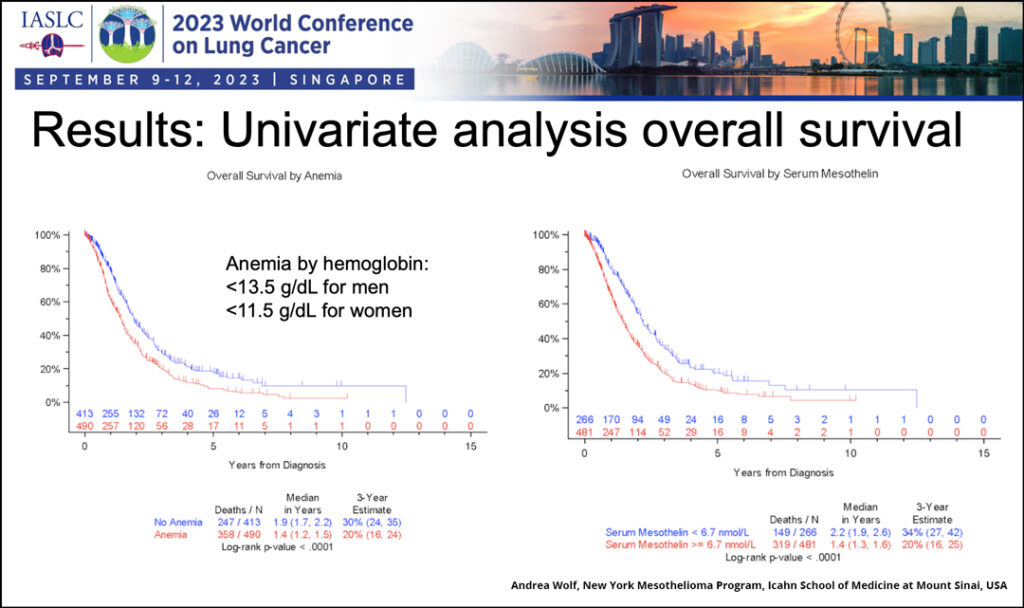
“We considered the previous analysis a training dataset and updated it with a more current, more clinically relevant cohort with less surgery,” said Andrea Wolf, MD, MPH, Associate Professor of Thoracic Surgery and Director of the New York Mesothelioma Program at the Icahn School of Medicine at Mount Sinai, New York. “On univariate analysis, anemia and mesothelin above an absolute cut point of 6.7 nmol/L were associated with worse survival.”
Dr. Wolfe presented “The IASLC Pleural Mesothelioma Staging Project: Updated Modeling of Prognostic Factors in Pleural Mesothelioma” as part of a mini oral session, Current Standards and Future Directions in Mesothelioma, on Tuesday, September 16. The session can be viewed on demand by registered WCLC 2023 attendees through December 31.
Overall survival was assessed by age, sex, histology, platelet count, white blood cell count, curative surgery, neoadjuvant and/or adjuvant therapy, and hemoglobin. Two additional variables were also assessed: anemia normalized to sex and mesothelin levels. Dr. Wolfe shared the overall survival data for the two additional variables, which showed them to be prognostic for worse survival (see figure).
For the multivariate analysis, which included all variables, two models were evaluated—a pathologic staging model based on clinicopathological features and treatment and a presentation model based on parameters typically available at patient presentation. The multivariable models were compared using Harrell’s c-index, where 0.50 is equivalent to chance and 0.70 is a good indicator of superiority.
In the pathologic model analysis, lack of neoadjuvant/adjuvant treatment, elevated platelet count, anemia, non-epithelioid histology, and stage III/IV disease were all associated with worse survival. Multivariate analysis of the presentation model showed non-epithelioid histology, anemia, elevated mesothelin, elevated platelets, and age >50 were associated with worse survival.
The c-index for the training cohort pathologic staging was 0.680 and 0.650 for the validation cohort. Adding anemia to the validation cohort boosted the c-index to 0.652 while adding mesothelin had no effect. The c-index for the validation cohort basic presentation was 0.668 compared to 0.550 for European Organization for Research and Treatment of Cancer (EORTC) pathologic staging criteria and 0.577 for EORTC basic presentation.
“Anemia is a strong predictor of worse survival,” Dr. Wolf said. “The IASLC models performed well compared to other models, but there is room for improvement. There is a clear need for standardized collection of data and for the collection of additional molecular biomarkers to improve our prognostic models. More accurate upfront staging is crucial for our patients.”