Thousands of Americans each year learn that CT chest screening has identified nodules on their lungs and, as a result, they often experience distress, fear, and confusion about their cancer risk, which may be compounded by miscommunications with their providers.
Theresa Roelke, MSN, APRN-AGPCNP, a nurse practitioner who specializes in geriatrics and manages the lung screening program at Maine Medical Center, thought a visual tool would increase clarity for this population, so she commissioned a 3D lung-nodule model that patients could study and touch during conversations with their care teams.
The model not only won a 2020 Innovator Award given by the Association of Community Cancer Centers but was featured during the “New Tools and Resources” portion of the IASLC’s 2021 CT Screening Symposium. Ms. Roelke spoke about the tool in a video shown at CTSS and in a second video produced by Maine Health for the Innovator Awards.
“(Research) showed that people were really anxious about lung nodules and felt they didn’t have a working knowledge of what it all meant in terms of not only sizing but content: What is this made up of? Is it an early cancer? Could it develop into cancer?” Ms. Roelke said.
Providing Tangible Understanding
To create her intervention, Ms. Roelke reached out to the Maine College of Art because the college had a 3D printer. She was matched with a student, William Kittredge, who helped her develop a series of prototypes. After Ms. Roelke tested the tool during meetings with 31 patients, a final product was produced by the Maker Innovation Studio at the University of Southern Maine, which fosters collaborative innovation across healthcare, business, industry, and education to develop prototypes, software, 3D technology, video animation and augmented- and virtual-reality projects.
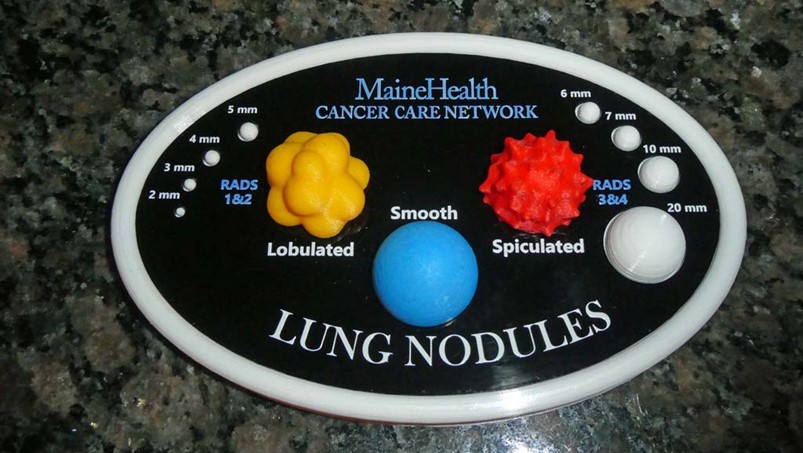
Lightweight and easy to fit into the pocket of a lab coat, the model is a flat board topped with 3D structures that illustrate the size of nodules ranging from 2 mm to 20 mm, along with their associated Lung-RADS scores. The board also incorporates structures that demonstrate the texture of lobulated, smooth, and spiculated lesions. Twenty copies have been made, and Ms. Roelke has applied for a grant that would allow other institutions to reproduce the model using their own logos.
In the clinic, she has found that “touching the nodules helps (patients) own the information about nodules in a tangible way which helps with recall. Patients have said, “A picture is worth a thousand words. When we can see something, engage with it, and touch it, we remember it far better.”
The model also “helps us reach out to the rural population that fits into our LDCT lung screening program,” Ms. Roelke said. “I have offered the tool across Maine Health to primary-care providers, pulmonologists, and emergency rooms, because a lot of nodules are found (as) incidental findings in the emergency department.”
Ms. Roelke urged other practitioners to consider using 3D printing to create other clinical tools.
“The possibilities are endless,” she said. “If you can sketch it out on paper, the tool can be developed. This is where art meets science to create innovations. It’s important to not only educate patients but educate providers.”